Understanding TMS Treatment: A Comprehensive Guide for Advanced Practice Nurses (APNs)
Transcranial Magnetic Stimulation (TMS) is emerging as a game-changer in the realm of mental health treatment, particularly for conditions like depression and anxiety. For Advanced Practice Nurses (APNs), understanding TMS treatment not only broadens their toolkit but also equips them to provide more comprehensive care. This article will explore the nuances of TMS treatment, its applications, and the role of APNs in this innovative field.
What is TMS Treatment?
Transcranial Magnetic Stimulation is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. Primarily utilized for treating major depressive disorder (MDD) in patients who have not responded to traditional treatments, TMS offers a novel approach to mental health care.
The Science Behind TMS
At its core, TMS operates on the principle of electromagnetic induction. A device generates magnetic pulses that can penetrate the skull and target specific areas of the brain, particularly the prefrontal cortex. This region is often linked to mood regulation. By stimulating the neurons in this area, TMS can help rewire neural pathways that contribute to depression and other mood disorders.
Benefits of TMS Treatment
The advantages of TMS treatment are manifold. One significant benefit is its non-invasive nature, which means patients don’t need anesthesia, and it typically involves minimal side effects compared to pharmacological options. Many patients report improvements in mood and overall functioning, often experiencing fewer episodes of depression.
Moreover, TMS can be administered in an outpatient setting, making it accessible to many individuals who may have difficulty adhering to more traditional treatment modalities. This ease of access is particularly important in mental health care, where barriers to treatment can often prevent individuals from seeking help.
Indications for TMS Treatment
While TMS is primarily associated with treatment-resistant depression, its applications are expanding. Recent studies indicate its effectiveness for other mental health disorders, including anxiety disorders, PTSD, and even OCD. As an APN, understanding these indications allows you to better assess and refer patients who may benefit from TMS.
The Role of APNs in TMS Treatment
Advanced Practice Nurses play a critical role in the implementation and management of TMS treatment. From assessing patient eligibility to providing ongoing support, APNs can significantly impact patient outcomes.
Patient Assessment and Eligibility
Before initiating TMS treatment, APNs must conduct thorough assessments to determine patient eligibility. This includes evaluating the severity of depressive symptoms, previous treatment history, and any contraindications. It’s essential to identify patients who are likely to benefit from TMS, as this can significantly enhance treatment efficacy.
A comprehensive assessment should also encompass the patient’s mental health history, co-occurring disorders, and any medications they are currently taking. By understanding the complete picture, APNs can make informed decisions and tailor treatment plans to individual needs.
Education and Counseling
Education is a cornerstone of effective patient care. APNs must provide patients with detailed information about the TMS procedure, including what to expect during sessions, the duration of treatment, and potential side effects. This not only helps alleviate patient anxiety but also promotes adherence to treatment.
Counseling is equally vital. APNs can offer emotional support and encouragement throughout the treatment process, helping patients navigate any challenges they may encounter. Building a trusting relationship is crucial, as many patients may feel apprehensive about trying a new form of therapy.
Collaboration with TMS Specialists
In many cases, APNs may work alongside TMS specialists or psychiatrists to ensure a cohesive treatment plan. Collaboration can enhance the overall patient experience, as specialists can provide additional insights and expertise in the technical aspects of TMS.
Effective communication between all members of the healthcare team is essential. Regular case discussions can facilitate a deeper understanding of patient progress and any necessary adjustments to the treatment protocol.
Understanding the TMS Procedure
The TMS procedure itself is relatively straightforward, but understanding each step can help APNs prepare their patients better and address any concerns that may arise.
Initial Consultation
The journey begins with an initial consultation, where the patient’s medical history and mental health status are thoroughly reviewed. During this meeting, the TMS specialist will explain the procedure, answer questions, and address any misconceptions the patient may have.
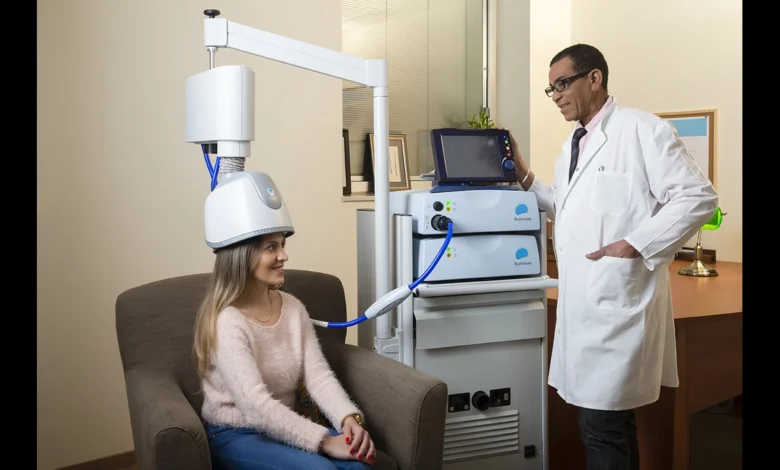
Treatment Sessions
A typical TMS treatment session lasts about 20 to 40 minutes. Patients are seated comfortably while a magnetic coil is placed against their scalp. The machine is then activated, delivering targeted magnetic pulses to stimulate the brain.
Most patients remain awake and alert during the procedure, and many report feeling only mild discomfort. It’s crucial for APNs to remind patients that they can communicate with the TMS technician throughout the session, making the experience more comfortable.
Frequency and Duration of Treatment
TMS treatment usually involves multiple sessions, typically five times a week for several weeks. The exact number of sessions can vary depending on individual patient needs and responses to treatment. APNs should encourage patients to attend all scheduled sessions to maximize the potential benefits of TMS.
Effectiveness of TMS Treatment
TMS has garnered significant attention for its effectiveness, particularly for those who have not found relief with conventional therapies. Research continues to support its use, demonstrating substantial improvements in patient outcomes.
Clinical Research and Findings
Numerous clinical studies have shown that TMS can lead to significant reductions in depressive symptoms. For instance, a meta-analysis published in a leading psychiatric journal highlighted that nearly 50% of patients achieved meaningful symptom relief after completing a TMS protocol.
Furthermore, research suggests that the benefits of TMS may extend beyond immediate symptom relief. Some studies indicate that patients experience sustained improvements in mood and functioning even after completing treatment, making TMS a compelling option for long-term mental health management.
Patient Experiences
Patient testimonials often reveal a profound sense of relief and hope following TMS treatment. Many individuals who have struggled with chronic depression express gratitude for the opportunity to regain control over their lives. APNs can play a pivotal role in helping patients share their experiences and connect with others who have undergone similar treatments.
Comparative Effectiveness
While TMS is not a one-size-fits-all solution, it offers a valuable alternative for patients who may not tolerate or respond to traditional antidepressants. By comparing the effectiveness of TMS with other treatment modalities, APNs can help patients make informed decisions about their care.
Side Effects and Safety Considerations
Like any medical treatment, TMS is not without its risks and side effects. Understanding these can help APNs provide comprehensive care and address any concerns patients may have.
Common Side Effects
The most frequently reported side effects of TMS are mild and temporary. These can include headache, scalp discomfort at the site of stimulation, and fatigue. It’s essential for APNs to inform patients that these side effects are generally manageable and tend to diminish with subsequent treatments.
Rare but Serious Risks
While serious side effects are rare, they can occur. The most notable risk associated with TMS is the potential for seizures, particularly in individuals with a history of seizure disorders. APNs must thoroughly evaluate patient histories and discuss any relevant concerns during the initial assessment.
Additionally, patients should be monitored closely throughout the treatment process. Regular check-ins can help identify any emerging issues early, allowing for timely interventions if necessary.
Precautions for Special Populations
Certain populations may require special considerations when undergoing TMS treatment. For example, individuals with implanted medical devices (like pacemakers) may need to be evaluated more carefully, as the magnetic fields could interfere with their devices.
APNs should also consider age, overall health, and concurrent mental health conditions when assessing suitability for TMS treatment. A collaborative approach with specialists can ensure that all safety measures are adhered to.
Integrating TMS into Holistic Care Plans
TMS should not be viewed as a standalone treatment but rather as a component of a broader, holistic approach to mental health care. For APNs, integrating TMS into comprehensive care plans can enhance treatment outcomes and provide patients with well-rounded support.
Complementary Therapies
Combining TMS with other therapeutic modalities can yield positive results. For example, cognitive-behavioral therapy (CBT) can complement TMS by addressing maladaptive thought patterns. This integrative approach can provide patients with tools to manage their mental health more effectively.
Additionally, lifestyle modifications, such as exercise, nutrition, and mindfulness practices, can support mental health and enhance the benefits of TMS. Encouraging patients to adopt a holistic lifestyle can be an invaluable part of their treatment journey.
Ongoing Monitoring and Support
Once TMS treatment concludes, ongoing monitoring is crucial. APNs should schedule regular follow-ups to assess patient progress and address any lingering symptoms or concerns. These check-ins can help patients feel supported and reduce the risk of relapse.
Providing resources for additional support, such as support groups or online communities, can further empower patients to take charge of their mental health. As APNs, fostering an environment of ongoing support can make a significant difference in patient recovery.
Long-Term Outcomes and Maintenance
Finally, considering the long-term outcomes of TMS treatment is essential. APNs can guide patients in developing maintenance strategies to sustain the benefits achieved during treatment. This may involve periodic TMS “booster” sessions or incorporating other therapeutic interventions as needed.
By emphasizing the importance of long-term care, APNs can help patients build resilience and maintain their mental well-being over time.
Future Directions in TMS Research
The field of TMS is evolving rapidly, with ongoing research exploring its potential applications and effectiveness. For APNs, staying informed about these advancements is key to providing cutting-edge care.
Innovations in TMS Technology
Recent innovations in TMS technology are making treatment more effective and accessible. Newer devices with improved targeting capabilities allow for more precise stimulation of specific brain regions, potentially enhancing treatment outcomes.
Additionally, advancements in TMS protocols, such as Theta Burst Stimulation (TBS), promise shorter treatment sessions with comparable effectiveness. This evolution in technology could increase patient compliance and improve overall treatment experiences.
Conclusion: The Future of TMS Treatment and APNs
Transcranial Magnetic Stimulation represents a significant advancement in mental health treatment, particularly for those who have struggled with traditional therapies. For Advanced Practice Nurses, mastering the nuances of TMS can enhance their practice and improve patient outcomes.
As TMS technology and research continue to evolve, APNs will play a crucial role in implementing these advancements. By prioritizing patient-centered care, dispelling misconceptions, and engaging in ongoing education, APNs can empower their patients on their journey toward mental wellness.
TMS treatment is not just a procedure; it’s a transformative experience that offers hope to many individuals. By embracing this innovative approach, APNs can contribute to a brighter future in mental health care, where patients receive the support they need to thrive.
you may also read
usainfotime.com